Overview of Dementia with Lewy Bodies disease:
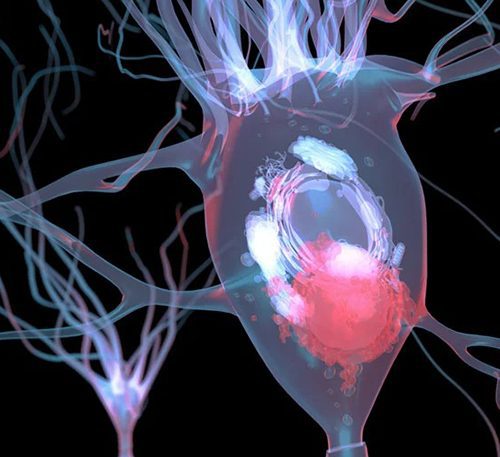
Dementia with Lewy Bodies (DLB) is a progressive neurodegenerative disorder that shares characteristics with both Alzheimer’s disease and Parkinson’s disease. It is characterized by the presence of abnormal protein deposits, known as Lewy bodies, in the brain. These deposits disrupt normal brain function, leading to a range of cognitive, motor, and psychiatric symptoms. DLB is considered the third most common cause of dementia, following Alzheimer’s and vascular dementia.
One of the distinguishing features of DLB is the presence of visual hallucinations early in the disease. Additionally, individuals with DLB often experience fluctuations in alertness and attention, which can lead to episodes of confusion and disorientation. Motor symptoms, akin to those seen in Parkinson’s disease, such as stiffness, tremors, and slow movements, are also prevalent in DLB. This complex combination of symptoms makes accurate diagnosis and appropriate management crucial for individuals affected by this challenging condition.
What are 3 signs of Lewy body dementia?
1. Visual Hallucinations and Fluctuating Alertness: One of the hallmark signs of Lewy body dementia (LBD) is the presence of vivid and recurrent visual hallucinations. Individuals affected by LBD may see things that others do not, which can be distressing and confusing. These hallucinations often involve people, animals, or objects and may contribute to feelings of disorientation. Additionally, LBD is characterized by fluctuating alertness and attention. This means that affected individuals may experience periods of relative clarity and coherence, followed by sudden episodes of confusion or drowsiness. These fluctuations can be unpredictable and may be exacerbated by stress or fatigue.

2. Parkinsonism Symptoms: LBD shares similarities with Parkinson’s disease, and individuals with LBD often exhibit Parkinsonism symptoms. These may include muscle rigidity, tremors, and a shuffling gait. These motor difficulties can lead to challenges in mobility and coordination. It’s important to note that while Parkinsonism symptoms are a common feature of LBD, not everyone with LBD will necessarily develop them, and the severity can vary from person to person.
3. Cognitive Impairment and Executive Dysfunction: Another key characteristic of LBD is cognitive impairment, which can encompass a range of difficulties with thinking, memory, and problem-solving. People with LBD may struggle with tasks that involve planning, organization, and decision-making, known as executive functions. This can impact daily activities and may lead to frustration or a sense of helplessness. It’s worth noting that cognitive symptoms in LBD can sometimes overlap with those seen in Alzheimer’s disease, which can complicate diagnosis. However, in LBD, cognitive changes often occur alongside the visual hallucinations and motor symptoms mentioned earlier, helping to differentiate it from other types of dementia.
What is the definition of dementia?
Dementia is a broad term used to describe a group of cognitive disorders characterized by a decline in mental abilities that significantly impairs a person’s daily functioning. It represents a spectrum of conditions, each with its own specific set of symptoms and underlying causes. The hallmark feature of dementia is a notable impairment in cognitive functions, such as memory, language, problem-solving, and the ability to focus and reason. This decline goes beyond what might be considered a normal age-related forgetfulness. Dementia is a progressive condition, meaning that symptoms tend to worsen over time, impacting various aspects of a person’s life.
In addition to cognitive decline, dementia often brings about changes in behavior, mood, and personality. Individuals with dementia may experience shifts in their emotional responses, ranging from irritability and anxiety to apathy and depression. These alterations can sometimes be challenging for both the individual affected and their caregivers. Furthermore, dementia can lead to difficulties in performing routine activities of daily living, like dressing, bathing, and preparing meals. As the condition advances, individuals may require increasing levels of support and care.
It’s important to note that dementia is not a specific disease itself, but rather a collective term encompassing various specific types of neurodegenerative conditions. Alzheimer’s disease is the most common form of dementia, accounting for a significant majority of cases. Other types include vascular dementia, Lewy body dementia, frontotemporal dementia, and more. Each type of dementia has its unique set of characteristics, underlying pathology, and progression patterns. Early diagnosis and appropriate management are crucial for providing individuals with dementia and their families the best possible quality of life and support.
What are the first symptoms of Lewy body dementia?
Lewy body dementia (LBD) can present with a range of early symptoms that may vary from person to person. One of the hallmark signs is visual hallucinations, where individuals affected by LBD may experience vivid and often recurring visual disturbances. These hallucinations can involve seeing people, animals, or objects that are not actually present. It’s important to note that these hallucinations are very real to the person experiencing them, which can be distressing and confusing. Additionally, LBD is characterized by fluctuations in alertness and attention. This means that individuals may have moments of relative clarity followed by sudden episodes of confusion or drowsiness. These fluctuations can be unpredictable and may be exacerbated by stress or fatigue.

Another common early symptom of Lewy body dementia is Parkinsonism, which includes motor difficulties similar to those seen in Parkinson’s disease. This can manifest as muscle rigidity, tremors, and a shuffling gait. These physical challenges can impact mobility and coordination, making everyday tasks more difficult. While not everyone with LBD will necessarily develop Parkinsonism symptoms, they are a distinguishing feature of the condition.
Cognitive impairment is another key indicator of LBD, though it can sometimes be subtle in the early stages. This can involve difficulties with thinking, memory, and problem-solving. Tasks that require planning, organization, and decision-making—collectively known as executive functions—may become more challenging. It’s worth noting that cognitive symptoms in LBD can sometimes overlap with those seen in Alzheimer’s disease, which can make diagnosis complex. However, in LBD, these cognitive changes often occur alongside the visual hallucinations and motor symptoms mentioned earlier, helping to differentiate it from other types of dementia. Recognizing these early signs is crucial for seeking timely medical evaluation and support.
What causes Parkinson’s disease dementia?
Parkinson’s disease dementia (PDD) is closely linked to the presence of abnormal protein deposits known as Lewy bodies. These Lewy bodies, which are primarily composed of a protein called alpha-synuclein, accumulate within nerve cells in various regions of the brain. In PDD, these deposits tend to accumulate not only in the substantia nigra—the area most affected in Parkinson’s disease—but also in other brain regions responsible for cognitive function. This widespread distribution of Lewy bodies disrupts normal cellular communication and function, leading to the cognitive decline characteristic of PDD.
The exact mechanisms underlying the formation of Lewy bodies and their role in PDD are still the subject of ongoing research. It is believed that abnormalities in the processing and clearance of alpha-synuclein play a crucial role. In individuals with PDD, there appears to be an accumulation of misfolded or aggregated alpha-synuclein, which eventually leads to the formation of Lewy bodies. These protein deposits interfere with the normal functioning of nerve cells, causing disruptions in neurotransmitter signaling and cellular communication.
Additionally, the spread of Lewy bodies through the brain appears to correlate with the progression of cognitive decline in PDD. As these abnormal protein deposits accumulate in regions associated with memory, attention, and other cognitive functions, it disrupts the neural circuits responsible for these processes. This disruption contributes to the cognitive impairments characteristic of PDD, including difficulties with memory, attention, problem-solving, and language.
Genetic factors may also play a role in the development of Lewy bodies and subsequently, PDD. Some individuals may have genetic predispositions that influence the accumulation and spread of alpha-synuclein. Environmental factors and other genetic variations could potentially interact with these predispositions, further influencing the progression of Lewy body pathology. Understanding the complex interplay of genetic and environmental factors in the formation of Lewy bodies is a crucial area of research in unraveling the underlying causes of Parkinson’s disease dementia.
What are the 7 stages of Lewy body dementia?
Lewy body dementia (LBD) progresses through a series of stages, each characterized by distinct patterns of symptoms and the accumulation of Lewy bodies in different regions of the brain. In the early stages, individuals may experience subtle cognitive changes, such as problems with attention, executive function, and visual perception. These early cognitive symptoms often precede significant motor symptoms typically associated with Parkinson’s disease. At this stage, the presence of Lewy bodies in the cerebral cortex, where higher cognitive functions occur, becomes increasingly prominent.
As LBD advances to the second stage, motor symptoms resembling Parkinson’s disease become more pronounced. These may include tremors, rigidity, and a shuffling gait. Alongside these motor difficulties, individuals may continue to experience cognitive challenges, including fluctuations in alertness and attention. Lewy bodies continue to accumulate in various brain regions, particularly in areas responsible for movement and cognitive processing.
The third and fourth stages of LBD mark a progression of both motor and cognitive symptoms. Motor function continues to deteriorate, with increased rigidity, slowed movements, and greater difficulties in coordination. Meanwhile, cognitive impairments become more apparent, affecting memory, problem-solving, and language. Individuals may also experience vivid visual hallucinations, a characteristic feature of LBD, as Lewy bodies further spread within the brain.
In the later stages of LBD, typically stages five through seven, the impact of Lewy bodies on an individual’s functioning becomes profoundly evident. Severe motor impairments make independent movement extremely challenging, often leading to wheelchair dependence. Communication may become limited, and individuals may require assistance with basic activities of daily living. The cognitive decline reaches a point where individuals may struggle to recognize loved ones and have difficulty articulating thoughts. Throughout these stages, the pervasive presence of Lewy bodies continues to disrupt brain function, profoundly affecting an individual’s quality of life. Understanding these stages is crucial for providing appropriate care and support for individuals and their families affected by Lewy body dementia.
How do you manage someone with Lewy body dementia?
Managing someone with Lewy body dementia (LBD) involves a multifaceted approach that addresses both the cognitive and motor symptoms associated with the presence of Lewy bodies in the brain. First and foremost, a comprehensive medical evaluation is essential for accurate diagnosis and to develop an individualized care plan. This may include assessments by neurologists, geriatricians, and other specialists experienced in treating Lewy body dementia. Medications targeting specific symptoms, such as those addressing cognitive decline or motor difficulties, can be prescribed to help alleviate some of the challenges posed by Lewy bodies.
Creating a supportive and structured environment is crucial in managing someone with LBD. Minimizing environmental stressors, such as excess noise or clutter, can help reduce agitation and confusion. Consistency in routines and familiar surroundings can provide a sense of security for individuals affected by Lewy body dementia. Additionally, ensuring safety within the home is paramount, as motor symptoms and fluctuations in alertness may increase the risk of falls or accidents. Modifying the living space to accommodate mobility aids or implementing safety measures, such as handrails, can help mitigate potential hazards.
Regular physical activity and exercises tailored to an individual’s capabilities can aid in managing the motor symptoms associated with Lewy body dementia. Engaging in activities that promote flexibility, balance, and strength can help improve mobility and reduce the risk of falls. Physical therapy and regular medical check-ups are important components of an overall care plan, allowing for ongoing assessment and adjustment of interventions to address the effects of Lewy bodies on motor function.
Providing emotional support and understanding is equally vital in managing someone with LBD. Caregivers and loved ones play a crucial role in providing reassurance, patience, and companionship. Offering a listening ear and maintaining open communication can help individuals cope with the cognitive and emotional challenges posed by Lewy body dementia. Additionally, seeking support from healthcare professionals and joining support groups specific to LBD can provide valuable resources and a sense of community for both individuals affected by Lewy body dementia and their caregivers.
What is the best medication for Lewy body dementia?
There isn’t a specific medication designed exclusively for treating Lewy body dementia (LBD). However, certain medications can be used to manage specific symptoms associated with LBD, which arise from the presence of Lewy bodies in the brain. Cholinesterase inhibitors, such as Donepezil, Rivastigmine, and Galantamine, are commonly prescribed to address cognitive symptoms like memory loss, confusion, and difficulties with thinking and reasoning. These medications work by increasing the levels of neurotransmitters that are important for cognitive function. By boosting communication between nerve cells, they can help mitigate some of the cognitive challenges posed by Lewy bodies.
In addition to cholinesterase inhibitors, other medications may be used to address specific symptoms related to motor function in LBD. Levodopa, a medication commonly prescribed for Parkinson’s disease, can be beneficial for managing the motor symptoms associated with the presence of Lewy bodies, such as tremors, stiffness, and difficulties with movement. Levodopa is converted in the brain into dopamine, a neurotransmitter that is deficient in individuals with Parkinsonism symptoms, including those with LBD. By replenishing dopamine levels, Levodopa can help alleviate some of the motor difficulties arising from Lewy body pathology.
It’s important to note that medication management for Lewy body dementia should be highly individualized. The choice of medication and dosage will depend on the specific symptoms an individual is experiencing, their overall health, and any potential interactions with other medications they may be taking. Regular communication with healthcare providers and close monitoring of the individual’s response to medication is crucial for optimizing treatment for Lewy body dementia. Additionally, it’s important to consult with a healthcare professional for the most up-to-date information on treatment options for Lewy body dementia, as research and guidelines may have evolved
What is the difference between Parkinson’s and dementia with Lewy bodies?
Parkinson’s disease and dementia with Lewy bodies (DLB) are two related but distinct neurodegenerative conditions characterized by the presence of Lewy bodies in the brain. While both conditions share common features, they manifest differently in terms of their primary symptoms and progression. In Parkinson’s disease, the initial and most prominent symptoms are motor-related, including tremors, rigidity, and bradykinesia (slowness of movement). The accumulation of Lewy bodies primarily occurs in the substantia nigra, a region of the brain crucial for motor control. In contrast, DLB presents with a combination of cognitive impairments, visual hallucinations, and Parkinsonism symptoms from the outset. Lewy bodies are distributed more widely in DLB, affecting both the cerebral cortex and areas responsible for movement.
Another significant distinction lies in the timing of cognitive symptoms. In Parkinson’s disease, cognitive changes typically occur later in the course of the illness, if they appear at all. These changes are often referred to as Parkinson’s disease dementia (PDD). In DLB, however, cognitive impairments are a central feature from the beginning. Memory problems, executive dysfunction, and visual-spatial difficulties are often evident early on, alongside visual hallucinations and Parkinsonism symptoms. This early and prominent cognitive involvement is a key factor that differentiates DLB from Parkinson’s disease.
Furthermore, individuals with DLB tend to experience more severe fluctuations in alertness and attention compared to those with Parkinson’s disease. These fluctuations can lead to sudden episodes of confusion, drowsiness, or even visual misperceptions. In Parkinson’s disease, such fluctuations are less pronounced. Additionally, individuals with DLB may exhibit more profound psychiatric symptoms, including mood changes, anxiety, and delusions. These features further contribute to the complex clinical picture of DLB, emphasizing the significant impact of Lewy bodies on both cognitive and psychiatric functions. Understanding these distinctions is critical for accurate diagnosis and tailored management of individuals affected by either Parkinson’s disease or dementia with Lewy bodies.
Conclusion:
In conclusion, Lewy bodies represent a defining characteristic in a spectrum of neurodegenerative disorders, including Parkinson’s disease and dementia with Lewy bodies. These abnormal protein deposits, primarily composed of alpha-synuclein, accumulate within nerve cells in various regions of the brain, disrupting normal cellular function. Their presence gives rise to a wide array of symptoms, ranging from motor difficulties and cognitive impairments to visual hallucinations and fluctuations in alertness. The distribution of Lewy bodies within the brain distinguishes conditions like Parkinson’s disease, where they predominantly affect areas linked to motor control, from dementia with Lewy bodies, where they are distributed more widely and significantly impact cognitive functions.
Research into the formation and impact of Lewy bodies continues to be a focal point in understanding and developing interventions for these debilitating conditions. Scientists are investigating the underlying mechanisms that lead to the aggregation of alpha-synuclein and exploring potential therapeutic strategies to prevent or mitigate Lewy body pathology. Additionally, advancements in diagnostic techniques are enabling earlier and more accurate detection of Lewy body-related disorders, facilitating timely interventions and personalized care.
As we deepen our understanding of Lewy bodies and their role in neurodegenerative diseases, there is hope for innovative treatments and interventions. The study of Lewy bodies not only sheds light on the complex pathology of these conditions but also paves the way for targeted approaches to alleviate symptoms and improve the quality of life for individuals affected by Parkinson’s disease and dementia with Lewy bodies. Ongoing research and collaboration in this field hold the promise of transformative breakthroughs, offering hope and support for those living with Lewy body-related disorders and their caregivers.
Related Links
FAQs:
Q: What Are Lewy Bodies, and How Do They Affect the Brain?
Answer: Lewy bodies are abnormal protein deposits primarily composed of alpha-synuclein. They accumulate within nerve cells in various regions of the brain, disrupting normal cellular function. Their presence leads to a wide range of symptoms, including motor difficulties, cognitive impairments, visual hallucinations, and fluctuations in alertness.
Q: How Does Lewy Bodies Differ from Other Neurodegenerative Conditions?
Answer: Lewy bodies distinguish conditions like Parkinson’s disease and dementia with Lewy bodies from other neurodegenerative disorders. In Parkinson’s disease, Lewy bodies predominantly affect areas linked to motor control. In contrast, in dementia with Lewy bodies, they are distributed more widely and significantly impact cognitive functions, leading to a distinct clinical presentation.
Q: Is There a Cure for Conditions Related to Lewy Bodies?
Answer: As of my last knowledge update in September 2021, there is no cure for conditions related to Lewy bodies. However, ongoing research is focused on understanding the underlying mechanisms and developing targeted interventions to prevent or mitigate Lewy body pathology. Treatment approaches primarily aim to manage symptoms and improve quality of life.
Q: Can Lewy Bodies be Detected in Living Individuals?
Answer: While definitive diagnosis of Lewy body-related disorders typically relies on post-mortem examination of brain tissue, advances in neuroimaging and biomarker research are showing promise in detecting Lewy bodies in living individuals. These emerging techniques hold potential for earlier and more accurate diagnosis.
Q: How Can Caregivers and Patients Find Support for Lewy Body-Related Conditions?
Answer: Numerous organizations and support groups are dedicated to providing resources, information, and a community for individuals and caregivers affected by conditions related to Lewy bodies. Healthcare providers, patient advocacy groups, and online forums can offer valuable guidance and a platform for sharing experiences and support.